Buvidal: An alternative to Methadone?
April 30, 2024
3:42 pm
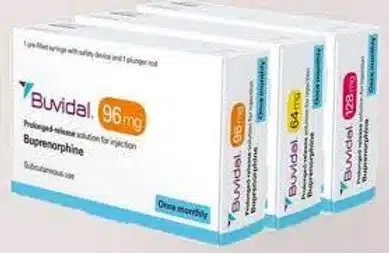
Buvidal is, quite simply, injectable Buprenorphine. It is given as an intramuscular injection, usually in the upper arm, and replaces the need to attend a chemist on a daily/weekly/ fortnightly basis. Different services have different protocols on how it will be prescribed. Ordinarily, it is given as a 16MG injection on week one, repeated for another four weeks and then as a monthly injection. But is Buvidal an alternative to Methadone?
As Buvidal is Buprenorphine, a patient needs to be in withdrawal before commencing treatment. While it is not dangerous to give it if someone is not, it will cause withdrawal as it will force opioids from the receptors in the brain. This is known as precipitated withdrawal. For those who have never used buprenorphine before, it is good practice to give the patient a small dose of oral buprenorphine, first, to ensure there are no issues. Thus a 4MG sublingual tablet or oral dispersable tablet is given. The patient would be asked to remain in the waiting room for an hour so any side effects could be measured/observed.
The usual practice is for clients to use oral buprenorphine (Subutex/Espranor) for two weeks, 1st, before moving to Espranor. This is to build on a therapeutic relationship and observe for adherence to treatment (urine drug screening). Also, Buvidal is somewhat cost prohibitive and a single injection can cost several hundred pounds. Oral Buprenorphine is, relatively, inexpensive.
While there are some obvious advantages to Buvidal such as no risk of diversion, assurance that the patient has had treatment, there are some considerations. Aside from the cost issue, already mentioned, there is also the issue that Buvidal does not provide the same “dampening” effect as Methadone. Dampening is when Methadone (when taken at therapeutic doses) stops someone feeling the effects when taking “on top” opioids (opioids in addition to Methadone).
While it is possible to have the injection a day or two either side of the due date, there is the risk that patients will stop engaging becuase it is an injection and it is “in their system.” However, and from what I have seen from my own experience of prescribing Buvidal, is that patients are expecting it to do things it simply can not do. In essence, it is not magic and is merely an injectable form of an existing drug: Buprenorphine. However, patients can be assertive in their demands to try it, especially when they are already on Methadone. And herein lies the most difficult problem.
Patients can only transfet to Buvidal when they are on 30MG of Methadone and coming down on Methadone is a marathon: not a sprint. A reduction of 2MG a week/fortnight is best and if a patient is on 100MG or more, this could take a year or more. Some clients will become overly focused on Buvidal and attempt to switch more quickly by either stopping their Methadone or reducing very quickly. This puts the patient at risk as their tolerance will drop and there is the additional risk of craving: A, potentially, dangerous combination. Furthermore. for clients who are alcohol dependent and/or using large amounts of gabapentinoids and benzodiazepines, Buvidal is not a realistic option as Naloxone will prove far less effective than it would against Methadone toxicity.
Clearly, treratment plans are made collabortatively between a patient and their clinician. For those who are not sensitive to Buprenorphine, Buvidal can provide a useful method of delivering Opioid Substiution Treatment (OST) , especially for those in rural areas and with complex, poly substance, dependencies. For satutory services, and fee paying patients alike, there are cost considerations and for those settled on Methadone, the risk of rapid termination of current treatment plans in order to transfet onto Buvidal.
Buprenorphine was first patented in 1965 and was licenced for use , in America, since 1981. It continues to be widely used for those with opioid dependency. Buvidal is,merely, the same drug in an injectable form. It, most certainly, has it’s uses but patients need to make an informed choice, in collaboration with their clinician and not nbe swayed by what they might hear from others or read on the internet.
Recent Posts

How Our Addiction Recovery Service Can Support Your Rehabilitation
Ready to start your journey towards recovery? Whether you’re looking for a residential rehab centre, or are interested in recovery at home, findmearehab.net can offer free and impartial advice. Our expert Paul provides a wide range of services to help you break free from addiction, including: Free and impartial rehab advice When looking to find…
Total SEO
2:05 pm, June 3, 2024

Get The Best Alcohol Addiction Treatment For Your Needs
One of the challenges of alcohol addiction is that it can be extremely complex, but it’s also highly treatable. However, treatments need to be tailored to the needs of the individual, and finding the best clinic is key for your recovery. Our clinicians provide advice on a range of issues, including information on alcohol addiction,…
Total SEO
4:36 pm, May 6, 2024

I don’t need drug and alcohol rehab! I can get a detox at home.
Let me start by saying that it is possible to do this, and I work with a consultant psychiatrist in addictions who can do this for you.
Admin
4:09 pm, April 30, 2024
